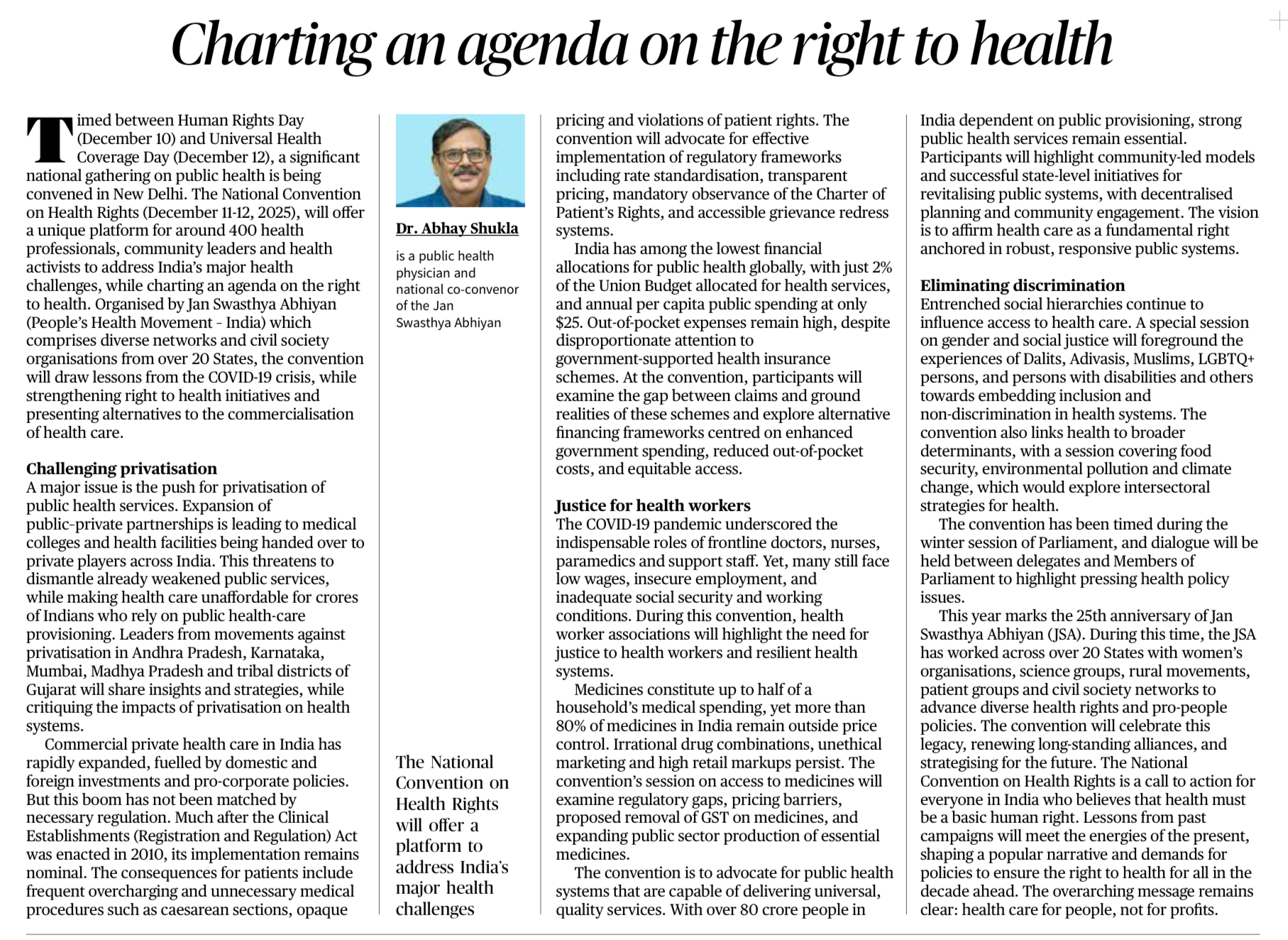
Context
• The National Convention on Health Rights (Dec 11–12, 2025) brings together health professionals and civil society from 20+ States to shape a national agenda on the Right to Health.
• Held around Human Rights Day and Universal Health Coverage Day, it reflects a push to strengthen public health systems post-COVID-19.
Key Issues Highlighted
A. Rising Privatisation of Healthcare
• Expansion of public–private partnerships and transfer of medical institutions to private players has made healthcare unaffordable.
• Despite the Clinical Establishments Act (2010), regulation remains weak → overcharging, unnecessary procedures, opaque pricing, violation of patient rights.
• Privatisation widens inequality as millions rely on weak public systems.
B. Low Public Financing
• India spends only 2% of the Union Budget on health and about $25 per capita annually — among the lowest globally.
• High out-of-pocket expenditure persists despite government insurance schemes.
• Convention will examine the gap between scheme promises and reality, and argue for higher public spending, equitable access, and reduced OOPE.
C. Justice for Health Workers
• COVID-19 revealed essential roles of doctors, nurses, ASHAs, paramedics.
• Yet they continue to face low wages, insecure contracts, poor working conditions, and inadequate social protection.
• The convention demands respect, fair pay, safety, and workforce strengthening to build resilient health systems.
D. Access to Medicines
• Medicines form half of household health spending.
• 80% of drugs in India remain outside price control → irrational pricing, unethical marketing, high markups.
• The convention advocates stronger price regulation, GST reform on medicines, and expansion of the public sector production of essential drugs.
E. Inclusion and Non-Discrimination
• Social hierarchies restrict access to care.
• A special session will highlight barriers faced by:
Dalits, Adivasis, Muslims, LGBTQ+ persons, persons with disabilities, and women.
• Emphasis on embedding equity and non-discrimination in health systems.
F. Public Provisioning & Community-Based Models
• Evidence from States shows that community-led, decentralised approaches can revitalise public health systems.
• The vision emphasises healthcare as a public good, not a profit-making commodity.
G. Broader Determinants of Health
• Links health to food security, environmental pollution, climate change.
• Calls for inter-sectoral collaboration for long-term health resilience.
Purpose of the Convention
• To push Parliament and policymakers toward Right to Health–based reforms.
• To resist commercialisation of health, reaffirming “healthcare for all, not profits”.
• Celebrates 25 years of the Jan Swasthya Abhiyan, showcasing its work with women’s groups, rural movements, and civil society networks.
TDF (Mains Question)
India’s public health system continues to face challenges of privatization, low public spending, inequity, and weak regulation. In this context, discuss the key concerns highlighted by recent debates on the Right to Health and suggest measures to strengthen public health systems. (150 words)